
Please Wait..

Please Wait..
|
|
|
|
The art and science of radiology became an integral part of veterinary medicine and surgery shortly after the exposure of the first radiographic film. The veterinarians are still not able to understand the real importance of radiology in their profession. When they properly apply it they will understand the importance of their profession. Among the special radiographic procedures, survey radiography remains the standard for the majority of ante-mortem anatomic diagnosis.
General terminologies:
1. Radiology: It is the branch of medical science which deals with diagnostic and therapeutic application of radiant-energy. Radiant energy are: X-rays, beta and Gamma radiations. It is also known as Roentgenology.
2. Veterinary Radiology: Branch of veterinary medical science which uses radiant energy principally for diagnostic as well as therapeutic purpose in domestic, companion, zoo and lab animals.
3. Radiologist: Any person qualified in medical/veterinary sciences and radiological physics to use radiant energy in the diagnostic, therapeutic and research field of medicine.
4. Radiograph: A visible photographic record in the film produced by X-rays passing through an object.
5. Radiographer: A technically trained/skilled person having the capacity to obtain quality radiographs for applied use by the radiologist.
6. X-rays: A special form of electromagnetic radiation, having high energy, extremely short wavelength, no mass or charge and travel at the speed of light.
Discovery of X-rays:
The discovery of X-rays was an accidental product of the work on the Crooke’s-type tube by Wilhelm Conrad Roentgen on 8th Nov- 1895. A professor of physics was working in laboratory at the Physical Institute of the Uni of Wurzburg, Germany, experimenting with a type of discharge or gas tube called Crooke’s-tube. He shielded the tube with heavy black cardboard. On shielding, he found that the greenish fluorescent light could be seen on a fluorescent screen kept 9 feet away. Roentgen concluded that a new type of ray was emitted from the tube that could pass through the black covering and that rays having the capacity to pass through most of substances but left the bones and most metal visible. After further investigation, Roentgen presented a written report to the society of physics and medical sciences at the University of Wurzburg on Nov-28 1895. With his findings, he also submitted a radiograph of his wife, Bertha’s hand with a ring, which he had produced with his own X-ray tube. By as early as April 1896, changes in skin color caused by exposure to X-rays, similar to sunburn, were reported. This discovery of skin color changes resulted in the use of X-rays for radiation therapy. In the recognition of roentgen’s discovery he was awarded the Nobel Prize in 1901 Dec-10. This was the first Nobel prize awarded in the field of Physics.
i. Name invisible rays as X-rays or unknown rays.
ii. discovered on Nov-8, 1895.
iii. Got Nobel prize on Dec 10 1901AD.
Historical background of Veterinary Radiology:
First oil emersed X-rays tube developed by Trowbridge.
Roentgen and colleagues made the first metal target X-rays tube.
First photographic paper developed for recording of X-rays image by Wright.
First radiograph made by Konig and Morten.
First veterinary radiograph of an equine foot published by Patan and Duncan in the March issue of veterinary journal.
Papers describing the use of X-rays in veterinary practice published by R. Eberlein and C. Troester of Germany , FTG Hobday, VE Johnson and J.A.W. Dollar of England and V. Lemoine of France.
3. 1897: AH Becquerel discovered radioactivity of Uranium.
J.J. Thomsan discovered electron.
4. 1898: Cannon used X-rays in the form of contrast studies (Wing bismuth meals) to investigate physiology of GIT.
5. 1901: Dec.10, 1901, W.C. Roentgen awarded 1st Nobel prize of Physics.
6. G. holtz Knecht developed first dosimeter for radiation therapy.
7. 1905: Kienbock was strips of silver bromide photographic paper to estimate dosage in radiation therapy.
8. 1913: Gustav Bucky invented grid to remove scatter radiation.
9. 1914: W.H. Bragg and W.L. Bragg discovered that X-rays would be reflected.
10. 1917: self rectifying generators developed for use in X-rays machine.
11. Early 1920’s:
12. 1928: International recommendations on radiation safety precautions were published.
13. 1930: Super voltage single section X-rays tube developed by C.C. Lauristan.
14. 1937: Xerox radiography invented by a physicist Chester F. Carlson.
15. 1945: Gray Schnelle wrote 1st American book on Veterinary Radiology.
16. 1950:
17. 1957: The organization of Educators in Veterinary radiology (EVRS) formed in USA .
18. 1972:
Possible uses of radiography in veterinary practice:
Production and properties of X-rays:
X-rays are electromagnetic radiations of high energy and short wavelength and are capable of penetrating the matter. Electromagnetic radiation is a method of transporting energy through space and is distinguished by it’s wavelength, frequency and energy. It behave as a particle as well as wave.
A. Wave characteristics:
|
Measured in Angstrom units |
Measured in meters |
||
|
Wavelength (A◦) |
Uses |
Wavelength (m) |
Uses |
|
Less than 1/10 |
Industrial radiology |
Close to 1/1000 m |
Microwave – RADAR |
|
1/10 to 1/2 |
Medical radiology |
Close to 1 m |
Television |
|
25 to 4000 |
UV-rays |
Close to 100 to 1000 m |
Communications |
|
4000 to 7700 |
Visible rays (VIGBYOR) |
Close to 10000000 m |
60 cycles AC |
|
7700 to 10000000 |
Infrared rays |
|
|
* Shorter the wavelength greater the penetrating power.
B. Electromagnetic radiation as a particle:
* Atoms consists of small particles called as protons, neutrons and electrons.
2. Production of X-rays:
 The following elements are necessary for X-rays production:
The following elements are necessary for X-rays production:
Processes involved:
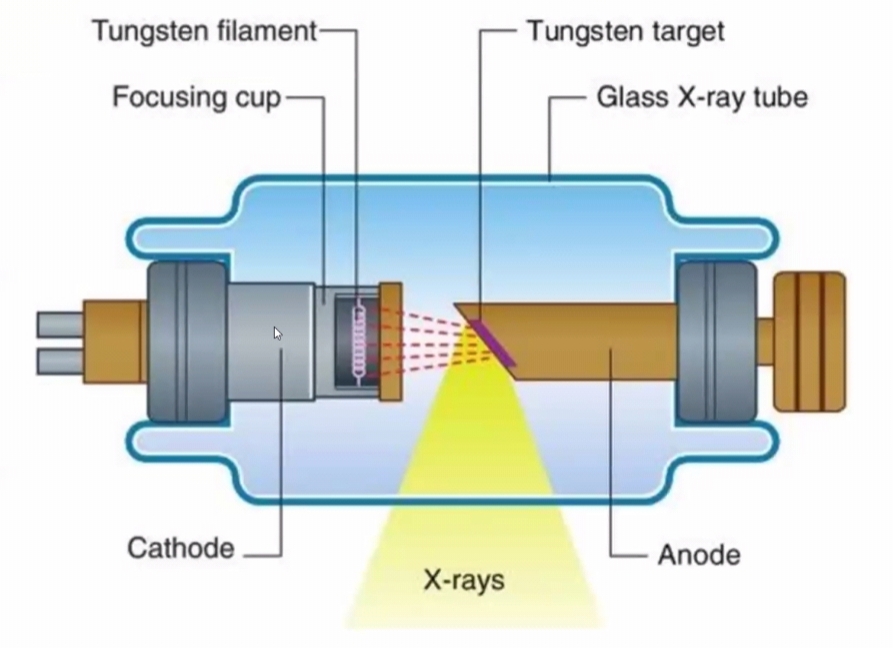
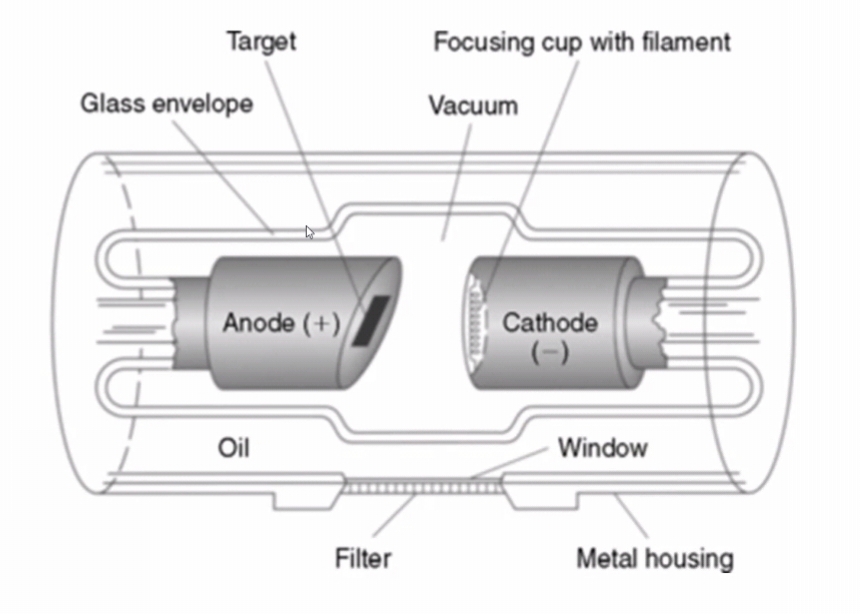
Cathode :
The negative side of the X-rays tube is called cathode. The purpose of the cathode is to provide a source of electrons and direct these electrons towards the anode. The cathode, assembly consists of filament and focusing cup.
i. Filament: the cathode consists of a coiled wire filament that emits electrons when heated. The filament in most X-ray tubes measures approximately 0.2 cm in diameter and 1 cm in length. It is mounted on rigid wires that support it and carry the electrical current used to heat the filament. The filament of the light bulb. Filament is made from the Tungsten having high melting point (3370◦C) and high atomic number. Small portable X-rays machine have a single filament. Most modern tubes have two filaments side by side: one being smaller than other with different capacity for heat and electron emission.
ii. Focusing cup: The filament is located in a concave cup called focusing cup. This cup is made from Molybdenum because it has high melting point and is poorer conductor of heat.
Anode:
Anode is the positive side of the x-rays tube. The target (anode) is composed of Tungsten which can withstand and dissipate high temperatures. The base of the target is made from copper. Copper acts as a conductor of heat and draws the heat away from the Tungsten target. Temperature in excess of 1000◦C is needed for X-rays production . Hence, the anode serves 2 main functions in the X-rays tube:
1. Provide mechanical support to the target
2. Acts as good thermal conductor of heat dissipation.
The anode in X-rays tube may be of two types:
1. Stationary anode: Used in dental, portable X-rays units, where high tube current and powers are not required.
2. Rotating anode: Used in X-rays units of larger capacity to produce high intensity X-rays beam in a short-time. The rotating anodes have better heat dissipation.
3. Properties of X-rays:
Working Principles of X-rays Machine and Radiographic Accessories:
(Filters, Restrictors, Collimators, Grid)
1. Portable X-rays Machines: Most commonly used in veterinary practices because of their convenient transportation. Such machines can be suspended from a rack or a strap or can be positioned on a wooded block. Portable machines are equipped with small sized low weight transformer located within the tube head. Small control panel is attached to the tube stand or supported on a separate stand. These machines have stationary anode with both single and double focal spot. The maximum output varies from 70-110 kV and 15-35 mA.
Advantages:
Disadvantages:
2. Mobile X-rays Machines:
Have higher output than portable machines by virtue of their larger transformers. Some models can be also useful for radiography of the digits in a standing animal. Usually, these machines have rotating anode with output of 90-125kV and 40-300 mA.
3. Fixed X-rays Machines:
Installed in a room especially constructed for the purposes. Large transformers are installed to have greater output. Output of these machines varies from 120-200kV and 300-1000 mA.
Advantages:
Disadvantages:
Technical Components:
A.Electrical components:
i. Transformer
ii. Timers
iii. Generators
B. Control panel:
Consists of:
1. On/ Off switch:
It is a main switch to turn the unit on. The switch permits flow of the current to the tube at ‘’On’’ position and prevents the same at the ‘’Off’’ position. For safety of the X-ray tube and also to avoid accidental exposure the switch remain in ‘off’ when machine isn’t being used.
2. Voltage compensator:
The voltmeter provides manual adjustment of the transformer to allow for inconsistent electrical output from the main electrical line. The line voltage should be checked whenever the machine is turned on. Most X-ray machines are designed to operate on a 220 voltage power source. In most machines these days such a system is automatic.
3. Kilo-voltage selector:
It allows precise selections of desired kV. Most modern X-ray machine are calibrated so that the desired value kV can be selected. However, in a number of smaller x-rays units the kilovoltage control is automatically linked with certain miliamperage.
4. Miliamperage selector:
The component let the radiographer select the desired current to cathode filament. This method of selection varies among X-rays machines.
5. Timer:
This mechanism allows the radiographer to pre-select the time of each exposure. The timer varies with models of x-ray machines. Example of timer include:
The advantage of the timer is the ability to use a short exposure time with accuracy.
6. Exposure button:
The exposure button is on the face of the control panel or attached to it by a length of cable. In either case the button should be in apposition to allow the person making the exposure to be at least two meters from the tube housing. Many X-ray machines operate on a two stage button. Two stages are necessary for the cathode filament to be activated and heated, to produce the electrons necessary for the exposure. Depression of first half of the button activates the filament and rotating anode, if present, and after few seconds, the button is fully depressed to complete the circuit for exposure.
7. Warning light:
Most control panel have light that illuminate when an exposure is made and x-rays are being emitted.
Radiographic accessories:
1. Filter
2. Restrictors
3. Collimators
4. Grid
5. X-ray film
1. Filter :
Composed of aluminium or Aluminium-copper, combinations absorbs low energy X-rays. The filtered x-ray beam decreases the exposure dose of the patient and scatter radiation. Primary purpose of placing a filter between the patient and x-ray tube is to remove less energetic (soft) x-rays from the primary beam.
2. Restrictors/ Cone:
Restrict field size. A small field size decreases the amount of the scatter radiation.
3. Collimators:
A restricting device used to control the size of the primary x-ray beam. The beam emerges from the x-ray tube in a diverging manner. If uncontrolled, the beam could extend to considerable width.
It serves to:
Several types of collimators are available which are placed in the path of x-ray beam as close the tube as housing permits. Following types of collimators are most commonly used:
Inherent filtration:
The absorption of x-rays by the x-ray tube and it’s housing is called inherent filtration.
In diagnostic x-ray tubes the glass is equal to about 0.5 mm Aluminium.
Added filtration:
Results from the absorbers(filters) placed in the path of x-ray beam.
Outside the x-ray tube and housing:
Thickness 1-1.5 mm aluminium equivalent. Can be customize (filter, thickness, type of metal).
Total filtration:
Total filtration = Inherent filtration + Added filtration
Recommended by NCRP:
|
Operating (kVp) |
Total filtration |
|
Below 50 kVp |
0.5 mm Al |
|
50-70 kVp |
1.5 mm Al |
|
Above 70 kVp |
2.5 mm Al |
4. Grid:
Position:
Pattern:
2. Crossed grid/ crisscross:
5. X-ray film:
How to take radiograph?
Dark room and radiographic processing
Principle steps of taking of radiograph:
A. Dark Room:
A-1 Light Proofing:
A-2 Floor
A-3 Painting and safe light:
Painting: Must be painted either with good quality paint of green or white.
Safe light: The maximum sensitivity of the x-ray film is in blue region of the spectrum, so the safe light should be amber green or red filter. Amber filter provides the maximum visibility with minimum fogging tendency.
Radiation protection:
Dark Room setting:
There needs two distinct work point in the dark room.
These two benches should be separated or kept apart by four feet. Preferably both sides are set on the opposite wall of the dark room. The workload is orderly sequenced. The equipment should be neatly placed in adequate space. When more than one person is working the movement of each person should have specific tract.
Dry bench:
Wet bench:
Processing of X-ray film:
Manual processing of the x-ray film:
It consists of five steps:
The developing of x-ray film:
Table: Time temperature variations:
|
Temperature (◦F) |
60 |
62 |
64 |
66 |
68 |
70 |
72 |
74 |
76 |
|
Time (Min) |
9 |
7.5 |
6.5 |
5.5 |
5 |
4*1/4 |
3*3/4 |
3×1/4 |
3 |
Composition of developer solutions:
* The pH of the solution is basic in nature.
Rinsing of the radiograph:
After a specified period in developer it should be taken out and then rinsed in water. The specified rinsing period is 30 seconds.
The composition of rinsing solution:
Fixing of the X-rays film:
The x-rays film should be placed in fixing solution and agitation of 15 seconds helps in prevention of streaking and staining of the finished solution. The removal of unexposed silver halide crystals is removed from the emulsion. For maximum hardening, the fixer takes 10 minutes. The time and temperature range is similar to that of developer i.e. optimum of 68◦F and ranged between 60-75◦F.
Comments:
Final washing of the x-rays film:
Adequate washing prevents dislocation and should be performed either in running water(30 minutes) or in stagnant water (2 hours). Frequent changing of the position of the film is rewardable.
Drying of the x-rays film:
After washing the film should be properly dried in open air or in automatically heated circulated air dryer.
Automatic processing of the X-rays film:
Factors affecting the production of radiographs:
# Make and type of x-ray machine:
A combination of kilovoltage, miliamperage and time setting that produces a satisfactory radiograph with one machine may not necessarily produce same quality of radiograph with another machine. The maximum output from different types of x-ray machine has been summarized as follows:
|
Type of x-ray machine |
kV |
mA |
mA×time (seconds) = 10 mAS |
|
Portable |
70-110 |
15-35 |
|
|
Mobile |
90-125 |
40-300 |
|
|
Fixed |
120-200 |
300-1000 |
|
Time should be always in the fraction of seconds.
# Incoming line voltage:
A fluctuation in the line voltage will allow consistent output. To be a consistent output the incoming line voltage should be fixed.
# Miliamperage and exposure time :
mAS mA×Time (s)
10 20×1/2
10 100×1/10
10 200×1/20
10 300×1/30
Advantages of maS:
# Kilovoltage:
kV determines the penetrability of the x-ray beam and thus affects the radiographic density (i.e. degree of blackness or whiteness on a radiograph). The potential difference between anode and cathode is measured in kilovoltage (1000 volt or kV). The kinetic energy of the electrons when they reach the target is proportional to the potential difference between cathode and anode. Hence, during an exposure time, the anode is maintained at high positive electrical potential relative to the cathode. Due to this difference in electrical charge, the electron cloud at filament is formed into narrow beam and accelerates the anode at very high speed. The kV determines the quality of the x-ray beam and it’s ability to penetrate.
There is an inverse relationship exists between kVP and mAS.
The kVP can be estimated by an equation known as Sante's rule, which states:
kVP= (2× thickness) +40
Where, the thickness of anatomical part in cm is measured by caliper and 40 represents focal-film distance in inch.
Eg.
Dr. ABC has requested an abdominal radiograph on a German shepherd dog. The measurement of lateral abdomen was 15 cm.
kVP = (2×thickness) + 40
= (2×15)+40 = 70 kVP has been to set.
# Distance:
FFD is the distance between focal spot in the target of the x-ray tube and the x-ray film. It is desirable to set optimum FFD for every radiographic exam. The most common FFD in veterinary practice ranges from 35 to 40 inches (90-100 cm). When different FFD is used, the adjustment of mAS can be calculated as:
New mAS = Old mAS × (new FFD/old FFD)²
Eg. = 10 mAS × (100/90)²
= 12.34 mAS
The distance between part to be exposed and x-ray film should be kept minimum as far as possible. To get good definition and avoid magnification, the PFD should be made Zero .
# Grid type:
A grid prevents radiation from falling on the film and thereby impress radiographic contrast (difference in densities in various part of the radiograph). It has been supposed that the use of grid requires increase in exposure factors. The increment depends on the ratio of grid.
Grid Increase exposure (mAS) by a factor of
5:1 2
8:1(used in vet) 3
12:1 4
# Type of film and intensifying screen used:
The intensified screen film requires 5 times less exposure as compared to non-intensified screen film.
# Thickness and nature of part to be exposed:
# Temperature and time of developing:
|
Temperature (◦F) |
60 |
62 |
64 |
66 |
68 |
70 |
72 |
74 |
76 |
|
Time (Min) |
9 |
7.5 |
6.5 |
5.5 |
5 |
4*1/4 |
3*3/4 |
3×1/4 |
3 |
Intensifying screen and it’s uses:
Intensifying screens interact with x-ray beam that has penetrated the patient and reached to the cassette. When the phosphor crystals in the screen are struck by the c-radiation: the crystal fluoresce whereby x-rays are converted into visible light. Remarkably, more than 95% of the exposure recorded in the film is due to light emitted from the intensifying screens. Only the remaining 5% of the exposure of the film results from ionization of the x-rays.
Efficiency of the screens material:
Construction of intensifying screens:
An intensifying screen has four integral layers with a total thickness of about 0.4 mm
1. A base or support:
The base serves as a flexible support to attach phosphor layer to the cassette. It is made either high grade cardboard or polyester. The base must have a tough moisture resistant surface and not become brittle with extended use.
2. A reflective layer:
This layer is closely attached to the base and is made of a white substance such as titanium dioxide. The purpose of the reflective layer is to reflect the light emitted by phosphor layer back towards the x-ray film.
3. A phosphor crystal layer:
This layer consists of uniformly distributed phosphor crystals held in the place with a binder material. The main function of it is to convert x-rays energy to visible layer. The materials to be used as phosphor crystals include:
4. a protective layer:
It is a transparent/clear layer placed on the outer surface of the screen.
Uses of intensifying:
Care of intensifying screens:
Rough handling leads to creation of the radioactive artifacts on the processed film. Routine inspection and cleaning of the screen should be done at least once in month. Following considerations should be remembered during care of the screens:
Uses of fluoroscopy:
It is used for a number of purposes:
Fluoroscopy (Adv. And Disadv.)
Fluoroscopy is essentially the visualization of a ‘’live’’ or ‘’real-time’’ radiographic image. It is a non-invasive procedure which uses x-rays to help capture and monitor video images of specific parts of the body while they are in motion.
Principles of fluoroscopy:
Advantages:
Dis-advantages
Contrast radiography:
Introduction:
Contrast is defined as the visible differences between two adjacent radiographic densities.
Divided into two separate categories: A. Radiographic contrast B. Subject contrast
A. Radiographic contrast:
i. Subject contrast ii. kVP level iii. Scatter radiation
iv. film type and v. Film fog
Basic radiographic opacities:
Radiographic image: it is produced when x-ray goes through the body part: Penetration and absorption.
Basic radiographic opacities:
If; Air= Black
Fat/ water= dark grey
Bone= Gray
Metal/ + contrast= Light gray
White
B. Subject contrast:
It is defined as the difference in density and mass between two adjacent anatomic structures, subject contrast is dependent on the thickness and density of the anatomical part. The body of the animal has many different types of tissues with variable densities. Some of the x-rays falling on a tissue get reflected, some others get absorbed, and only the remaining ones pass through the tissue. The more radiations penetrate through the muscle as compared to the bone, this is due to difference in density of beam caused by object is subject contrast. Bone absorbs most of the x-rays falling on it, soft tissue very little and air containing organs like lungs, bowel practically nil. Bone will absorb many more x-rays than muscle or fat, assuming both have equal thickness. With appropriate exposure factors, anatomy that has high tissue density can increase the amount of whites and blacks on the radiograph; therefore high subject contrast increases the radiographic contrast.
Contrast radiography?
Under normal circumstances, soft tissue structures or organs are difficult or impossible to identify on a plain films awing to lack of contrast. When the radio-density of the tissue itself or it’s surrounding structure is deliberately altered to obtain a radiograph with enhanced visualization and demarcation, it is called contrast radiography.
Advantages of contrast radiography:
Contrast medium:
A substance that is either radiolucent or radio-opaque that can be administered to an animal to increase radiographic contrast within an organ or syatem.
Types
Positive Negative
(BaSO4, Iodine-Ionic and water soluble) (CO2, Air, N2, NO2, O2)
1. Positive contrast media:
Materials which increase radio-density of the structure or tissue in relation to surrounding tissue are called positive contrast media. Barium or iodine preparation , contain element of high atomic number. Absorb more x-rays than do the soft tissues or bones. Radio-opaque to x-rays and appear white on a radiograph. Used to fill or outline a hollow organ (e.g. Urinary bladder, GIT) or injected into the blood vessels (sterile water based compounds only) for immediate visualization of vascular supply or for subsequent excretion evaluation.
2. Negative contrast media:
Materials having the property to increase the radio-density of the structure as compared to surrounding tissue are known as Negative contrast media. The substances having low specific gravity like room air, oxygen and carbon-dioxide are commonly used negative contrast media. Others are nitrogen and nitrous oxide. An ideal negative contrast media should be inert, quickly dissolved in fluid and quickly eliminated from the body. Substances with low specific gravity are more radiolucent to x-rays than soft tissues and have a black appearance on a radiograph.
Contrast agents:
1. Positive contrast agents:
I. Barium-sulfate preparations: medium of choice for radiographic studies if the GIT.
Because it is:
Forms: Liquid, paste and powder for reconstitution with water.
Indications:
Oesophagography, Gastrography, Reticulography, Barium enema, Barium meal for GIT
Contra-indications:
II. Iodine preparations: The iodine compounds are divided into two sub-categories: Water soluble agents and Viscous/ oily agent.
A. Water soluble agents: Make up the largest group of contrast agents. Most water soluble preparations are:
Administration of positive contrast agents:
These agents are injected into a vascular system for immediate visualization of the system or subsequent demonstration of the excretory system. In addition, water soluble agents can be infused into the urinary bladder via urinary catheter to visualize the urinary mucosa, bladder shape and size. In market, these water soluble agents are available in ionic or non-ionic form.
i. Ionic preparations:
Indications
Contra-indications:
Non-ionic forms: Metrizamide (Amipaque-30n) – for myelography, angiography and IV pyelography (renal pelvis)
2) Oily/ viscous agent:
Have limited application in veterinary radiography, only limited to lymphography. These can be used for myelography if non-ionic form isn’t available.
Negative contrast agents: E.g. Air, O2, CO2, N2, N2O
CO2 has an advantage over room air because CO2 is better absorbed into body into hollow organ, room air can cause air emboli. It is used for radiography of hollow organ (pneumocystography) and soft tissue.
3. Double contrast:
A radiographic contrast technique that uses a combination of the both positive and negative contrast media simultaneously. For example : to diagnose the foreign bodies in stomach- we have to administer both Barium meal as well as air. Urinary bladder to look for the presence of uroliths.
Principles of viewing and interpretation of x-ray film:
Viewing of Radiographs:
In order to evaluate a film completely, a radiograph should be viewed on and evenly lit view box in a semi-darkened room. The viewing box screen should be clean and light bulbs in working order. For obvious practical reasons, films are usually examined white it is still wet. However, wet film is swollen and as it dries it will contract and improve definition. Therefore, the radiograph for evaluating the lesions of fine detail, final examination should be postponed until radiographs dries properly. The standard radiographic viewing box has a screen measuring 17×14 inches, which is adequate for all normal radiographs. There is considerable advantage in having two viewing boxes or one with double size. So that at least two film showing suspected pathology with a normal of the same area or build up the three dimensional concepts of lesion from films taken in two different planes. In certain viewing boxes, the intensity of illumination can be varied, which facilitate the examination of films which vary in density. For areas of such density, some form of spot light may be necessary to show the details of such local areas. The light should not be too bright or strongly illuminated because it makes radiologist’s eyes to radiograph difficult. It can also be helpful to have magnifying glass when making a close inspection of films showing particularly fine detail. The position of film on the view screen is also important. Veterinary radiographers generally follow the medical protocol for viewing. Ventrodorsal or dorsoventral anatomy, such as abdomen or thorax, should be placed on the view screen so that animal is at top and patient’s right is on the viewer’s left. A laterally positioned anatomy should face the viewer’s left with spine at the top.
Interpretation of x-rays:
Radiographic diagnosis doesn’t depend on gross radiological appearances. Radiological appearances must be able to make a specific diagnosis of a particular condition. Good interpretation is an art and requires a careful pain staking approach to each film.
Basic concepts of interpretation of radiograph:
The radiographic image is a two-dimensional representation of a three-dimensional body part. Characteristic radiographic appearance depended upon it’s thickness form and atomic number.
Relative radio-densities:
Air, fat soft tissue bone, surgical pin
Radiolucent Radio-opaque
|
Tissue/ object |
Effective atomic number |
Physical density (sp. gravity) |
|
Gas |
1-2 |
0.001 |
|
Fat |
6-7 |
0.9 |
|
Soft tissue/ fluid |
7-8 |
1 |
|
Bone |
14 |
1.8 |
|
Metal (lead) |
82 |
11.3 |
Relative radio-densities:
The image is a summation of anatomic shadows. Interpretation of radiographs requires imagination and logical analysis. Radiographic interpretation is based on the visualization and analysis of opacities on a radiograph.
Radiologic interpretation:
Description of radiologic abnormalities (Roentgen signs):
Touquet’s ten commandments of emergency radiology:
Command :
Rules of Two for interpretation:
Interpretation of x-ray films:
Each films should be examined noting every structure or tissue that can be :
Significant variation from the normal will be indicated by one or more of the following features:
Displacement of the structure:
This may show the pathology of an adjacent organ (upward displacement of trachea can be indicative of- Enlargement of a mediastinal lymphatic gland) or the structure itself (e.g. a displaced hip)
Variation of density of tissue:
The density may be:
Break or variation in contour: A break or variation in contour of the part (fracture, neoplastic enlargement of an organ). Variation in the detailed structure of the part or tissue (juvenile osteoporosis).
Classification of the radiographic lesions:
After examination of the dry diagnostic radiograph, the lesions can be classified as :
Radiographic lesions can be seen as abnormal size, shape, location, magnification, density or absence of an organ or tissue.
Systemic lesions:
The entire radiograph should be examined systemically. Systemic methods include examination of each system (musculoskeletal , pulmonary, cardiac, gastro-intestinal etc.).
Pathological lesions:
Radiographic lesions can be seen as normal size, shape, location, magnification, density or absence of an organ or tissues.
It can be further categorized as: i. Degenerative ii. Infectious iii. Anomalous iv.Neoplastic v. Iatrogenic
Key points:
Radiotherapy:
Introduction:
Treatment of the diseases by means of Roentgen rays or other forms of the radioactivity. These therapies are mostly indicated to treat rapidly dividing malignant and non-malignant tumors. Radiation therapy for the treatment of neoplasms of the domestic animals has been used since discovery of x-rays. Dr. R. Eberlin of Berlin Vet. School was the first to report (1906-1912) on the use of radiotherapy in vet practice. It’s use in veterinary medicine in treating neoplasm has yet to be introduced in Nepal. Radiation therapy has been stalled due to expenses involved and alternatively, the chemotherapy is widely used.
Indications of radiotherapy:
Sources of the radiation exposure:
A. Natural radiation exposure
1. Cosmic rays
2. Environmental
i. Terrestrial
ii. Atmospheric
3. Internal radiation
B. Artificial radiation exposure
1. Cosmic rays:
Originate in outer space and pass through atmosphere. At normal living altitudes, exposure 35 mrad/year. At altitudes above 20KM cosmic radiation becomes important.
2. Environmental:
i. Terrestrial radiation: Radioactive element such as thorium, uranium, radium and isotopes of potassium (K40). Exposure: 50 mrad/year.
ii. Atmospheric radiation: from radioactive gas as Radon, Thoron. Exposure: 2 mrad/year
3. Internal radiation:
i. Include minute quantities of uranium, thorium and related substances.
ii. Isotopes of K40, Strontium (Sr99) and C14.
Exposure: 25 mrad/year
Non-occupational radiation sources:
1. Radon = 56% 2. Manmade = 17%
3. Terrestrial = 8% 4. Cosmic = 8%
5. Internal = 11%
B. Artificial Radiation Exposure:
4. Miscellaneous: Television set, Radioactive dials, Watches, Isotopes, Tagged products, Luminous markers.
Types of radiation:
1. Electromagnetic radiation:
Radio waves, micro-waves, infrared, visible light, ultraviolet, x-rays, Gamma rays. These all are the same form of energy-the only differ in the amount of energy packets (photons) that they contain.
Characteristics:
2. Corpuscular radiation: It has low penetration power. E.g. µ-rays, b-particles( electrons) and photons.
|
Types of radiation |
Approximate penetrating ability |
||||
|
|
Air |
Tissues |
Lead |
||
|
µ-particles |
4 cm |
0.05 mm |
0 |
||
|
b-particles |
6-300 cm |
0.06-4.0 mm |
0.005-0.3 mm |
||
|
g-rays |
400 cm |
50 cm |
0.3 mm |
||
|
x-rays |
120-240 cm |
15-30 cm |
0.3 mm |
||
|
|
Cosmic rays |
Some components very high |
|||
Alpha particles:
Physical characteristics:
Range: 1-2 inches in air
Shielding: Dead layer of skin
Biological hazards: Internal , it can deposit large amount of energy in a small amount of body tissue.
Alpha-particles are highly energetic Helium nucleus.
Beta- Particles:
Physical characteristics:
Range: Short distance( one inch to 20 feet)
Shielding: Plastic
Biological hazards: Internal hazards. Externally, may be hazardous to skin and eyes.
Gamma-rays/ X-rays:
Physical characteristics:
Range: Very far.
Shielding: Concrete, water, lead
Biological hazards:
Mechanism of action of radiation:
The mechanism by which cells are killed by ionization isn’t fully understood. Two theories are postulated in this regards-
1. Direct or target theory
2. Indirect theory
Direct or target theory:
The radiant energy acts by direct hit on the target molecules within the cells. To ionize the molecules, either single or multiple hits are required.
During this process, energy gets deposited within the molecules which is greater than the binding energy of the electrons.
This results in ejection of the orbital electrons, a change in chemical configuration of the molecule and thus damage to the cells.
DNA molecules in the primary target for radiation induced cell death (especially linkages and bonds within the DNA molecules)
Ionizing radiation generates free radicals and receives oxygen intermediates that damage local cellular constituents especially DNA.
DNA double strands breaks are critical lesions that result in cell death.
Depending upon the radio-sensitivity of the tissues, dose, and duration of the radiation, there are three principal effects on the DNA molecules.
Principal effects on the DNA molecules:
Indirect theory:
This theory proposes that the energy exerts it’s effects by producing free ‘hot’ radicals, such as peroxides within the cell that damage the specific target.
Water molecules the major constituents of the cell and get ionized into H+ , OH- and other unstable particles such as HO2 and H2O2.
Since these radicals are highly unstable, they react rapidly among themselves and others solutes within the solution producing a crucial biological change in the cell which leads to cell death.
#Radiation effects on biological tissues:
Methods of radiotherapy:
Radiotherapy shortens the cell division and hence increases the number of cells. This is achieved by 4 R’s radiotherapy:
Radiotherapy is never done by a single dose; rather multiple treatments are given over a period of time, termed fractional therapy. In animals, it is usually done in 10-12 fractions of radiation dose of 4-5 Gy each time, usually three times per week.
During fractioned therapy:
Methods:
A. Tele-therapy:
The radiation is kept at a distance from a lesion. It is of four types:
B. Brachy-therapy:
In this radio-sensitive materials are placed in direct contact with tissue being treated. Sources are usually in the form of surface applicators- needle, seeds or grains etc.
Particularly useful in treating the cancer of:
Specific method of brachy-therapy:
a) Interstitial brachytherapy:
E.g. Au(198), Co (60) etc. are placed within the interstitium of the neoplasm.
Advantages:
Dis-advantages:
b) Plieso-therapy (surface) : e.g. use of Sr(90) for superficial lesions.
c) Systemic brachytherapy: I (131) and P (32) can be administered systemically.
What is radio-isotopes?
The isotopes are those nuclides which
Isotopes of elements may be:
Unstable nuclides undergo the process of decay to form stable nuclides by the process of radioactive decay.
Ultrasonography (USG):
Principle:
Electricity
Transducer
Ultrasound waves
Tissue
Image
Introduction:
USG is a unique imaging modality for the soft tissue structures of the body. It has been routinely used in human medicine as well as in veterinary practice abroad. It is an important imaging modality in vet medicine since 1980 AD. USG, when used will be the new addition of diagnostic modality. In Nepak, it is not used popularly due to lack of technical know- how and facilities.
Ultrasound is defined as sound waves of frequencies greater than audible to the human ear i.e. greater than 20,000 Hz. Frequencies between 2 and 10 MHz are mainly used for diagnostic ultrasound.
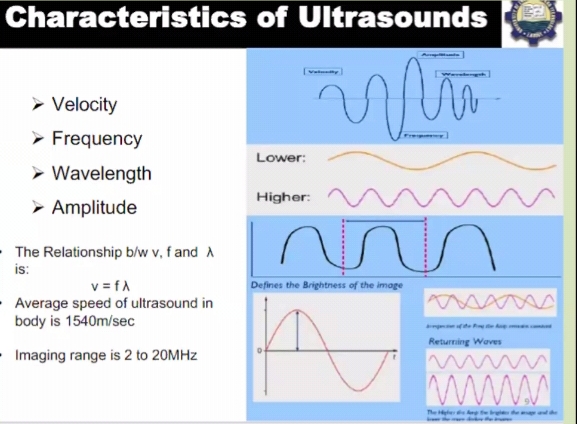
Selection of frequencies is inversely proportional to the depth of the tissue from the scan surface. A sound wave travels in pulse and when it is reflected back it becomes an echo and this pulse-echo principle is used for ultrasound imaging. Intensity of the returning echoes is expressed as brightness in the display is known as ultrasonography. Ultrasound can provide information about the organ architecture independent of organ function. It is especially helpful in debilitated or very young patients, in which:
Ultrasonographic findings are not necessarily as specific as histological diagnosis. However, the ability to distinguish solid masses from those contained fluid.
Principle:
The ultrasound has been used to produce an image or photograph of an organ or tissues and echoes are recorded as they strike tissues of different densities. USG is a diagnostic procedure using sound-waves. The ultrasonographic machines produce sound having velocity 1540 m/s. Sound waves like light rays are governed the laws of reflection and refraction. The amount of reflection and refraction while passing through the structures depends on:
Interaction of ultrasound with tissues:
1. Reflection: Occurs at a boundary between 2 adjacent tissues or media. Acoustic impedance (z). the ultrasound image is formed from reflected echoes.
2. Transmission: Not all the sound wave is reflected, some continues deeper into the body. These waves will reflect from deeper tissue structures.
3. Scattering: Redirection of sound in several directions, caused by interaction with small reflected or rough surface. Only portion of sound wave returns to transducer.
4. Attenuation: The deeper the wave travels in the body, the weaker it becomes. The amplitude of the wave decreases with increasing depth.
* The miss-match between the different structures in a given part of the body provides their differentiation in imaging.
*Maximum information is provided when the beam hits the imaging structures at 90◦ angle.
Ultrasound production:
Transducer contains:
Procedures of ultrasound:
Parts of USG machine:
1. Transducer
2. CPU
3. Key board
4. Display
5. Storage device
6. Printer
# How is an image is formed on the monitor?
Advantages:
Disadvantages:
Indications:
Principle of Physical Therapy, it’s Classification, Scope and Limitations
Physical therapy is a technique to increase the mobility and function of joints and
muscles in animals. This technique can reduce the pain and enhance the recovery from
injury, disease, degenerative disease, age related disease and obesity. The main goal of
therapy is to increase the quality of life and decrease the pain. Each technique used in
animal physical therapy has different benefits and not all techniques are useful for all
conditions.
Classification: There are different types of physical therapy. Some of them are followings:
1. Massage
2. Hydrotherapy
3. Cryotherapy
4. Heat therapy
5. Passive range of motion
6. Balance therapy
7. Walking therapy
8. Cavalleti rails
9. Land treadmill
1) Massage: It is used in animals to relieve tension in muscles and stimulate muscle development. It speed up recovery from injury and surgery by increasing the blood flow to the area and relieving muscle spasm. It is generally used in canine physical therapy and used to improve the comfort in animals in all conditions.
2) Hydrotherapy: This technique uses water as a tool to improve the muscles and joint functions in animal. Underwater treadmill is commonly used in animal physical therapy. It provides benefits of land exercises decreasing the weight placed on the animal`s limb allowing them to ambulate and perform specific exercise due to buoyancy of water. It is very useful in dogs recovering from surgery such as anterior cruciate ligament and cranial cruciate ligament repairs and break repairs.
Benefits : Indications:
3) Cryotherapy: Cryotherapy (or cold therapy) is the application of a cold agent to an affected area of the body, such as a surgical site, to provide therapeutic effects by reducing tissue temperature. Cryotherapy is found to be effective in the first 72 hours after acute injury or surgery.
Benefits:
Indications:
It is used in any injury or procedure that causes inflammation, pain, or decreased range of motion and neurologic disorders, such as spasticity. Specific surgical procedures where cryotherapy is indicated postoperatively for pain and swelling include:
4) Heat therapy: Heat therapyexert effects opposite to that of cryotherapy. however, both modalities are used to provide analgesia and decrease muscle spasms but the timing of application are different. Since cold therapy should be performed for the first 72 hours, heat therapy should only be initiated after 72 hours and continued for a period based on the individual patient, typically 5 to 7 days. Beginning heat therapy too early can lead to worsening edema, swelling, and potential seroma formation.
Benefits:
Indications:
5) Passive range of motion: Passive range of motion (PROM) refers to exercises that move joints through their available range of motion without weight bearing muscle contraction.
Benefits:
6)Balance therapy: It can be used to improve balance once the patient has regained the ability to stand on its own or with the assistance of a sling or therapy ball. This therapy is focused on helping the animal to understand that the affected limb is no longer painful.
Benefits:
Indications:
7) Walking therapy: It is beneficial and applicable to any rehabilitation program.
Benefits:
Indications: Indicated in early rehabilitation of animals refusing to use their affected limb due to muscle weakness, decreased range of motion, circulation disorders, neurologic deficits, and proprioceptive deficits.
Walking exercises may improve:
8) Cavalleti rails: Cavalletti rails are rails that are raised above the ground a certain
distance for patients to walk over.
Benefits include increasing stride length, range of motion, proprioception, balance, and limb use.
Indications:
9)Land treadmills: Treadmill walking are used in reducing pain, making the patient bear weight on the affected limb to strengthen muscles, increasing proprioception and range of motion, producing a normal gait, and providing cardiovascular and endurance benefits.
Indications:
Scope of physical therapy:
1. Examining (history, system review and tests and measures) individuals in order to determine diagnosis, prognosis, and intervention.
2. Alleviating impairment and functional limitation by designing, implementing, and modifying therapeutic interventions.
3. Preventing injury, impairment, functional limitation, and disability, including the promotion and maintenance of fitness, health, and quality of life in all species of animals.
Limitations:
1. Takes longer time period
2. More costly
3. Continuous effort is required
4. May cause accidental hazards.
Computed Tomography (CT) scan
CT scan utilizes rotating X-rays around the part to be examined to make cross-sectional. Both 2 and 3- Dimensional images are reconstructed from the acquired CT data around a single axis of rotation.
Advantages:
Disadvantages:
Magnetic Resonance Imaging (MRI)
It is a medical imaging technique to visualize internal structures of the body by using the property of nuclear magnetic resonance to image nuclei of atoms inside the body.
Advantages:
Disadvantages
Diathermy:
Mechanism of action:
Diathermy uses very high frequencies (0.5-3 MHz) of electrical current. This allows diathermy to avoid the frequencies used by body systems generating electrical current, such as skeletal muscle and cardiac muscle, allowing body physiology to be broadly unaffected during it’s use.
The radiofrequencies generated by the diathermy heat the tissue to allow for cutting and coagulation by creating intracellular oscillation of molecules within the cells. Depending on the temperature reached different results occur:
At 60 – cell death , 60-99 – dehydration and tissue coagulate and at 100 – tissue vapourises (Temp is in degree celsius).
Indications:
Contraindications:
Scintigraphy (Nuclear Medicine)
Radio-isotopes are used to detect functional status of the body systems.
Principle based on: Use of a pharmaceutical labeled with an isotope that after entry into the blood stream gets localized in a particular tissue or organ.
The localization of the isotopes can be then detected by using a detector or gamma camera due to emission of gamma rays from the area of interest.
Sodium iodide crystal is used which absorb gamma rays emitted by radio-isotope from the organ and converts it into light flushes.
A computer system is usually attached to the camera for gathering data and it’s display and quantification.
Most commonly used isotope is Technitium-99
Pharmaceuticals for organ imaging (e.g. pyrophosphate or methylene diphosphate for bone, macro-aggregated albumen for lung perfusion)
A scan appears as an image formed of dot. The interpretation is based on the appearance of increased (hot spots) , decreased (cold spots) radioactivity regions.
Advantages:
Disadvantages:
Weekly updates
Apr 27, 2024
Weekly updates
Apr 27, 2024
Weekly updates
Apr 27, 2024